Ages ago, doctors didn’t have the ability to image structures so they relied heavily on careful detailed written description to accompany hand drawn diagrams to monitor their patients. Sounds archaic doesn’t it? Living in 2014, we now have a breadth of tools that can help us see structures in the body that we can’t even see with the naked eye – if given the choice of a hand drawn picture with written notes versus an advanced diagnostic image of the organ in question, which would you prefer to have done? What if it could save your vision or your life? With current electronic medical record keeping, there often isn’t an option to draw so a detailed description is usually the only option we doctors have to document your condition. Depending on the space in the patient record that 1 or 2 sentence description of the part of the body is used to remind the doctor a year or two later what she or he saw at the previous visit and make clinical decisions on the health status of that particular part of your body. Does that worry you?
Ages ago, doctors didn’t have the ability to image structures so they relied heavily on careful detailed written description to accompany hand drawn diagrams to monitor their patients. Sounds archaic doesn’t it? Living in 2014, we now have a breadth of tools that can help us see structures in the body that we can’t even see with the naked eye – if given the choice of a hand drawn picture with written notes versus an advanced diagnostic image of the organ in question, which would you prefer to have done? What if it could save your vision or your life? With current electronic medical record keeping, there often isn’t an option to draw so a detailed description is usually the only option we doctors have to document your condition. Depending on the space in the patient record that 1 or 2 sentence description of the part of the body is used to remind the doctor a year or two later what she or he saw at the previous visit and make clinical decisions on the health status of that particular part of your body. Does that worry you?
Can you imagine your dentist NOT taking an x-ray to monitor your or your child’s oral health and development? Relying on written word to describe the anatomy to make clinical decisions in 2014? Considering everyone with a smartphone is capturing their living history by snapping away at everything from the breakfast they eat to the party last night, it seems like our memory is getting worse or at least we are less willing to rely on them.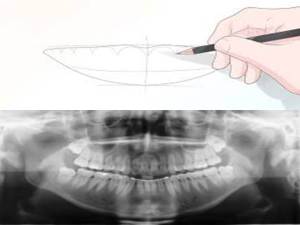
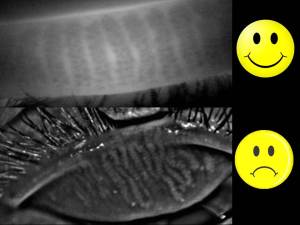
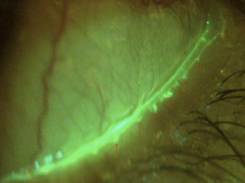
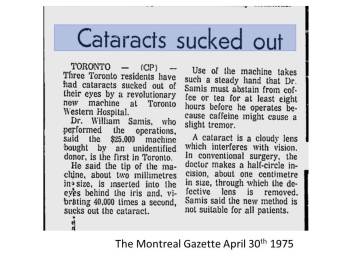
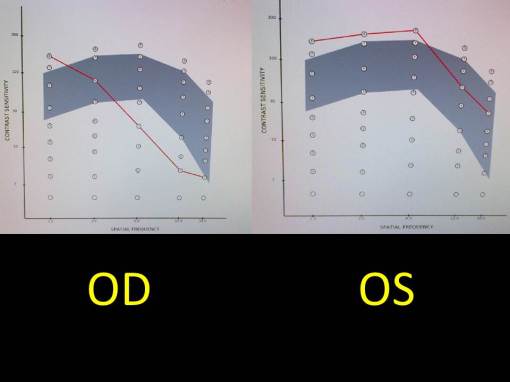
The organ I look after is the eye, and there are several areas of the eye that require careful and detailed attention to changes in size, thickness, elevation, artery angles, reflectivity, etc. (I could go on). With the advances in technology, imaging the eye is now possible such that we can even see through the tissues and assess what is not visible under a microscope or to the naked eye. We can now track discrete changes down to a fraction of a hair using digital quality images and video so that the slightest change becomes part of the patient record for generations to come. We can invert, flip, and virtually turn the eye inside out in order to assess potential holes, bleeding, retinal detachments, etc. Gone are the days where we to rely on deciphering our written notes from a year ago to monitor for change – or are they?
Depending on where you live, these types of images are not covered by government insurance plans and even some private plans. Their lack of coverage however doesn’t make them any less relevant to your ocular health. In fact it is a well accepted science that imaging the optic nerve, retina and other ocular structures provides earlier diagnosis and better overall management.  With an image set, your eye doctor can review areas over and over with scrutiny without having to subject the patient to holding their eye open with a bright light being blasted at them. It takes away the issue of patient movement while examining the eye, which makes it extremely difficult to provide an accurate and efficient assessment. For children this is particularly helpful. With this combined information of an image set and your doctors microscopic evaluation, this provides you with the most comprehensive assessment using 21st century technology.
With an image set, your eye doctor can review areas over and over with scrutiny without having to subject the patient to holding their eye open with a bright light being blasted at them. It takes away the issue of patient movement while examining the eye, which makes it extremely difficult to provide an accurate and efficient assessment. For children this is particularly helpful. With this combined information of an image set and your doctors microscopic evaluation, this provides you with the most comprehensive assessment using 21st century technology.
What is astounding to me is that despite what we know about the relevance and importance of the diagnostic eye imaging, there are still some patients that don’t seem to understand its utility and choose to not have it done – like opting out of a warranty at Best Buy. With all advances in technology, very few have failed to adopt; do you still use a VCR or an 8-track tape player to watch your movies or listen to music? If my mechanic requests that I run a diagnostic on my car, I generally rely on her or his professional judgement to decide on having that test done. I can’t think of the last time I said “no’ to a dental x-ray. In general I rely heavily on the experience of my service providers to recommend what is best.
My patients are educated thoroughly on why I make this type of diagnostic choice in order to provide the most thorough of eye care. Prevention and wellness are as much a part of health care as the treatment we provide for what ails you. In fact, identifying earlier and intervening before major damage has set in can save your vision for years to come. Diabetes for example doesn’t have to cause blindness. With regular comprehensive eye examinations and retinal diagnostics, we can actually prevent this disease from taking your vision away. Countries like the UK that have a national program employing such diagnostics are actually seeing a stabilization in the number of diabetes related blindness after almost 10 years of implementation.
So why are we opting out in North America of retinal diagnostics despite what eye doctors know to be the best way to preserve your most precious of senses? Why don’t we provide the most comprehensive care on 100% of patients? Have we commoditized eye care and the value of our doctor’s extensive clinical training and experience? Do patients value vision the same way we negotiate for a car? For the sake of all of our eyes – I hope not.
In good health,
Dr. Richard Maharaj OD, FAAO
Cinical Director,
eyeLABS Optometry and Center for Ocular Surface Disease
twitter: @eyelabsinc
info@eyelabs.ca