Fear. The word itself causes one to take pause and hold back. For doctors, fear of litigation likely tops the list of reasons to refer patients out but fear of making a disease worse has historically allowed half truths about treating anterior eye disease to thrive. For instance the fear behind using a topical steroid by both family medicine and even ophthalmology and optometry has hindered its use to this day – even when it is indicated for treatment. This article will discuss a specific ‘sore’ spot in the eye bank, HSV and HZO, and the role of topical steroid administration in quelling this persistent nemesis.
HSV is carried by 90% of people, however most remain dormant and don’t show up in our exam chairs. When they do however, red flags and alarm bells immediately start to ring because the ability of this bug to thrive has caused corneal scarring and blinded many since its first human to human identification by Vidal in 1893. Although patients assume sexual transmission when they hear “herpes,” eye related infections are often not primary and therefore not sexually transmitted at all. The stigma, like the virus, has survived despite our best efforts.
The inflammatory stage of herpes simplex keratitis occurs because of the coating of the virus itself produced from this clever virus’ protein coding. One protein in particular similar to human corneal protein is called UL8 which triggers an immune response. Because UL8 is similar the normal corneal proteins, the immune system begins to attack healthy tissue in addition to the virus itself, triggering CD4+ T cells which release chemokines and Th1 cytokines resulting in a destructive inflammatory cascade. Other supposed sources of inflammation are CD8+ T cells which are more destructive and lead the corneal scarring that has come to be associated with HSV end stage.
Epithelial Involvement:
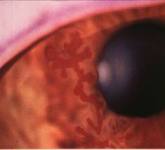
Differentiating is key. Epithelial involvement can be small or large lesions with that typical dendritic appearence, but without a terminal bulb glowing with an additional vital dye (Rose or Lissamine), it can be easily misdiagnosed. If you don’t have an additional dye and are convinced of bulbs then back up your diagnosis with corneal sensitivity testing. Dental floss – the old nylon type – or even a cotton tip that has been teased out can serve as an vital tool at confirming your diagnosis. Test the good eye first and then the affected eye. The aesthesia score will be markedly reduced and this is a positive diagnosis of HSK. Clinical history will generally agree with these 2 test results.
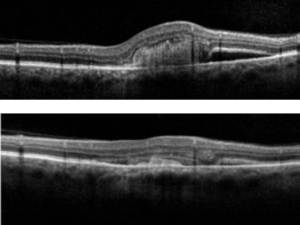
Interstitial Keratitis vs. Endotheliitis:
Stromal or interstitial keratitis (immune mediated) will be just that – limited to the stroma and will NOT involve the epithelium or the endothelium. A thin beam on your slit lamp will help to isolate the haze and only in this isolation can you diagnose as interstitial. Often misdiagnosed as interstitial keratitis is the disciform lesion. A true disciform lesion (without epithelial invovement) will ALWAYS involve the endothelium and is in fact an endotheliitis. HSV endotheliitis comes in 2 other forms diffuse, and linear, based on the pattern of endothelial dysfunction and stromal edema. Typically this is accompanied by an anterior chamber reaction and elevated IOP second to trabeculitis.

Of course, with epithelial involvement the use of a steroid is contraindicated however doctors should not fear or hesitate its use in cases with intact or non-necrotizing epithelium. Interstitial HSK and endotheliitis require a topical corticosteroid administered in addition to oral antivirals to suppress the immune response. Now that said, we’ve all been burned by a case in the past so what will happen if a steroid is applied to an epithelial case? This is where your clinical judgement and direction is key. Follow up in 1-3 days and clearly instruct this patient that should vision or symptoms change for the worse at all, to call the clinic immediately or head to urgent eye care if after hours. An incorrect use of steroid on a small missed lesion will not cause the eye to explode but will serve as a provocative test. Yes the lesion will expand and the virus will accelerate shedding. I’m not condoning or advising the use of steroid to diagnose HSV, however I will follow that by saying it is a manageable ship to turn around with topical antivirals, (zirgan is very effective) provided it gets caught early and managed aggressively.
Topical Treatment:
HSV keratitis:
- Viroptic (trifluiridine) q2H x 1 wk or until epithelium is healed and thereafter qid x 1 wk.
- Zirgan (gangcyclovir)5x daily x 1wk or until epithlium is healed and thereafter tid x 1 wk
Zirgan is an excellent new additional to the arsenal and friendly to the ocular surface.
Oral Treatment:
- Zovirax (acyclovir) 400mg five times daily for seven to 10 days
- Valtrex (valacylovir) 500mg three times daily for seven to 10 days
- Famvir (famciclovir) 250mg three times daily for seven to 10 days.
HZO keratitis:
- Zovirax (acyclovir, GlaxoSmithKline) 800mg five times daily for seven to 10 days.
- Valtrex (valacylovir, GlaxoSmithKline) 1,000mg three times daily for seven to 10 days
- Famvir (famciclovir, Novartis) 500mg three times daily for seven to 10 days.
Interstital or Endotheliitis:
Add topical steroid (lotemax or prednisolone have demonstrated equivalent efficacy) q1-2h and taper appropriately as resolved which can be for weeks or months. This is extremely key in reducing the immune response. Without topical steroid it can persist and prolong viral shedding and even increase the risk of necrotizing and or scarring.
Now this certainly isn’t an A-Z coverage on HSV or HZO – geographic and neurotrophic ulcers are both noteable subsets which generally occur in chronically untreated or misdiagnosed cases and have extreme visual consequences. I’ve chosen to reserve that discussion for another thread. Managing the ocular surface is always paramount so Viroptic preserved with thimerasol is certainly a thorn, which is why Zirgan offers a better and more effective alternative. Of course lubricate with preservative free drops during this period and be careful to instruct about drop insertion. If the patient is doing what you’ve instructed, the only reason the keratitis will persist is because they are poking themselves with the dropper tip and causing their own keratitis!
Dr. Richard Maharaj OD, FAAO
Director of Optometry,
eyeLABS Inc.
twitter: @eyelabsinc
rmaharaj@eyelabs.ca






 As the content of our textbooks become outdated keeping up with current opinions in eye care can be daunting. Combined with that is a complacency that some doctors have that they will somehow stay current through osmosis. The reality is that keeping abreast of all the general and sub-specialties within optometry and ophthalmology is near impossible so when I stumble upon a GREAT resource, the educator in me must share it. Dr. Larry Alexander OD FAAO, a great friend and a pillar in the optometric community has started a wonderful website
As the content of our textbooks become outdated keeping up with current opinions in eye care can be daunting. Combined with that is a complacency that some doctors have that they will somehow stay current through osmosis. The reality is that keeping abreast of all the general and sub-specialties within optometry and ophthalmology is near impossible so when I stumble upon a GREAT resource, the educator in me must share it. Dr. Larry Alexander OD FAAO, a great friend and a pillar in the optometric community has started a wonderful website  The nutriceutical industry is bombarded with ‘miracle medicines’ claiming to cure all that ails you, however without any regulating body these over-the-counter non-prescription pills are too varied for the consumer to make sense of when faced with 5 feet of choices at your local superstore or pharmacy. Now, the reality is that some molecules actually do have merit and have been shown in repeated studies and world-renowned institutions like John Hopkins Hospital to have medical efficacy in a variety of conditions. In this article, I will reveal my top 3 picks for nutriceutical supplements for the eyes for 2013 and why. These picks are based on my research and my clinical work with these supplements. A little background here: I have worked with A LOT of supplements over my career and I have scrutinized claims made in scientific literature in clinical settings. I chose them after a detailed due diligence on my part and to be clear I have no financial interests or ties to any of the listed products.
The nutriceutical industry is bombarded with ‘miracle medicines’ claiming to cure all that ails you, however without any regulating body these over-the-counter non-prescription pills are too varied for the consumer to make sense of when faced with 5 feet of choices at your local superstore or pharmacy. Now, the reality is that some molecules actually do have merit and have been shown in repeated studies and world-renowned institutions like John Hopkins Hospital to have medical efficacy in a variety of conditions. In this article, I will reveal my top 3 picks for nutriceutical supplements for the eyes for 2013 and why. These picks are based on my research and my clinical work with these supplements. A little background here: I have worked with A LOT of supplements over my career and I have scrutinized claims made in scientific literature in clinical settings. I chose them after a detailed due diligence on my part and to be clear I have no financial interests or ties to any of the listed products.