Having practiced for over 10 years now, I’ve had the most success and most impact on my dry eye patients in the last 2 years. I just celebrated a milestone of having helped 200 patients achieve a level of clinical stability and symptomatic relief of their chronic dry eye disease. I attribute that success to the breadth of clinical knowledge and research that I’ve put into building the dry eye clinic in addition to the dramatic increased volume of peer reviewed science directed towards the study of dry eye disease and its causes. More than anything else, however I attribute my patients success to the cases that failed initial treatment. A good scientist’s successes are shouldered by his or her failures.
In this brief article I want to share from my dry eye cases that responded poorly or not at all to therapy. It’s funny but 3 specific cases always come to mind when I think about this subject. One case involves Lyme disease, another was a male with ‘borderline-normal’ testosterone and the last was a case of ‘he said she said’.
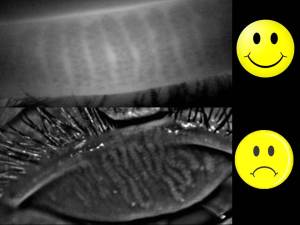
 1) Patient S.A. had been battling a diagnosis of Lyme disease when she presented to my office and all clinical signs pointed to MGD. Meibography showed mild truncation but nothing more than I had seen in my most successful cases, and they certainly had viable expression on forced palpation. Despite effective clearing of obstruction using LipiFlow (confirmed on post meibography) and improved ocular surface staining, she remained with mild improvement in meibum expression. Her symptoms, as often observed with dry eye disease failed to match the improved clinical picture. Systemically she was also not improving which I attributed to her lack of improvement. However on closer inspection corneal sensitivity pre-treatment and 6 months later had increased. I had assumed that initial testing was basal and normal, however it was more likely that this patient had experienced hypoaesthesia on presentation and treatment resulted in increased surface threshold sensitivity – a return to normal feeling if you will. Lesson: Longstanding cases of DED with and without systemic involvement will at some point undergo neural upregulation (or dysregulation) which can and will confuse the clinical picture. I’ve learned from this that staying the course in the interest of decreasing inflammation is prudent, despite a failing symptomatic picture. Sometimes feeling anything is better then feeling nothing at all!
1) Patient S.A. had been battling a diagnosis of Lyme disease when she presented to my office and all clinical signs pointed to MGD. Meibography showed mild truncation but nothing more than I had seen in my most successful cases, and they certainly had viable expression on forced palpation. Despite effective clearing of obstruction using LipiFlow (confirmed on post meibography) and improved ocular surface staining, she remained with mild improvement in meibum expression. Her symptoms, as often observed with dry eye disease failed to match the improved clinical picture. Systemically she was also not improving which I attributed to her lack of improvement. However on closer inspection corneal sensitivity pre-treatment and 6 months later had increased. I had assumed that initial testing was basal and normal, however it was more likely that this patient had experienced hypoaesthesia on presentation and treatment resulted in increased surface threshold sensitivity – a return to normal feeling if you will. Lesson: Longstanding cases of DED with and without systemic involvement will at some point undergo neural upregulation (or dysregulation) which can and will confuse the clinical picture. I’ve learned from this that staying the course in the interest of decreasing inflammation is prudent, despite a failing symptomatic picture. Sometimes feeling anything is better then feeling nothing at all!
 2) Patient M.H. had been to 3 corneal specialists in the previous 5 years. He had been on various doses of doxycycline, restasis, all artificial tears, plugs with little improvement and even less hope. The lid margin was hyperkeratinized and expression was low volume but clear. Without staining these lids, I could see why my 3 colleagues before me were frustrated. I proceeded with lid margin debridmenet/scaling technique by Maharaj Triad technique. Patient had mild relief lasting 3 days and symptoms returned to similar levels as previous. The brief improvement validated my approach so we proceeded twice more 1 month apart each. Each time relief was lasting longer but failing to provide any sustained comfort. Finally he mentioned how depressed this was getting him and how he had experienced sexual dysfunction that had been worsening over the last few years (he was late 30’s). On further questioning his energy had reduced greatly and he had been on and off anti-depressants. I promptly requested getting his testosterone measured by his family physician. This was the missing link and it proved to be a turning point in this patient’s disease state. Lesson: Men with dry eye disease with limited clinical signs should be screened for androgen insufficiency. Increasing this patient’s zinc intake and making some lifestyle changes had a significant impact on the ocular surface and meibum volume.
2) Patient M.H. had been to 3 corneal specialists in the previous 5 years. He had been on various doses of doxycycline, restasis, all artificial tears, plugs with little improvement and even less hope. The lid margin was hyperkeratinized and expression was low volume but clear. Without staining these lids, I could see why my 3 colleagues before me were frustrated. I proceeded with lid margin debridmenet/scaling technique by Maharaj Triad technique. Patient had mild relief lasting 3 days and symptoms returned to similar levels as previous. The brief improvement validated my approach so we proceeded twice more 1 month apart each. Each time relief was lasting longer but failing to provide any sustained comfort. Finally he mentioned how depressed this was getting him and how he had experienced sexual dysfunction that had been worsening over the last few years (he was late 30’s). On further questioning his energy had reduced greatly and he had been on and off anti-depressants. I promptly requested getting his testosterone measured by his family physician. This was the missing link and it proved to be a turning point in this patient’s disease state. Lesson: Men with dry eye disease with limited clinical signs should be screened for androgen insufficiency. Increasing this patient’s zinc intake and making some lifestyle changes had a significant impact on the ocular surface and meibum volume.
3) Patient TS. presented with severe symptoms and clinical signs of chronic mixed aqueous/evaporative DED. Meibography showed a unique pattern  of atrophy, however the majority of the ductule and acini were intact. She insisted on not having undergone any treatment other than some at home efforts with warm compresses and all the artificial tears on the market with little help from anything. Although the atrophy was atypical, I proceeded to clear the meibomian gland obstructions using LipiFlow in addition to lid margin debridement/scaling. All metrics showed that she should have overwhelming success. She did not. At month 1 her glands had not improved and there appeared to be increased keratinization at the margin accompanied by further atrophy and cicatricial changes. The patient had no history of viral conjunctivitis and I was officially stumped. She consistently returned to my clinic enthusiastic but always reserved and mixed up on her use medicines and on chronology of her appointments. I smelled deception. By probing further and being honest about my disappointment in her lack of success, she volunteered that she had undergone meibomian gland probing 2 weeks after having had LipiFlow with me. This explained everything. Lesson: Honesty is the best policy, but shouldn’t always be assumed. Patients can be deceptive for reasons of guilt, lack of understanding, overconfidence, or just plain confusion. When the clinical picture doesn’t fit for your dry eye patient, probe and question further. History is still the gold standard in choosing a path of treatment for these patients!
of atrophy, however the majority of the ductule and acini were intact. She insisted on not having undergone any treatment other than some at home efforts with warm compresses and all the artificial tears on the market with little help from anything. Although the atrophy was atypical, I proceeded to clear the meibomian gland obstructions using LipiFlow in addition to lid margin debridement/scaling. All metrics showed that she should have overwhelming success. She did not. At month 1 her glands had not improved and there appeared to be increased keratinization at the margin accompanied by further atrophy and cicatricial changes. The patient had no history of viral conjunctivitis and I was officially stumped. She consistently returned to my clinic enthusiastic but always reserved and mixed up on her use medicines and on chronology of her appointments. I smelled deception. By probing further and being honest about my disappointment in her lack of success, she volunteered that she had undergone meibomian gland probing 2 weeks after having had LipiFlow with me. This explained everything. Lesson: Honesty is the best policy, but shouldn’t always be assumed. Patients can be deceptive for reasons of guilt, lack of understanding, overconfidence, or just plain confusion. When the clinical picture doesn’t fit for your dry eye patient, probe and question further. History is still the gold standard in choosing a path of treatment for these patients!
Other tips:
1) Don’t wait to offer more than artificial tears and prescribed drops. These aren’t restorative treatments but are palliative in nature. Almost every patient I’ve treated has said, “I only wish I had this done sooner.” The average patient has been seen by 3 doctors prior to showing up at the dry eye clinic.
2) Follow through – what patients don’t tell you is that it’s just not working or that they’ve lost confidence in the ‘same old approach.’ Like the contact lens patient that has been fitted in monthly CL’s for years from their optometrist, they will leave if offered a more comfortable 1 day disposable by the nearest competitor and they won’t tell you about it. Tell your patients about new options for dry eye disease and give them a chance to say no.
3) Don’t let a patient become refractory to treatment! A 50+ female wearing makeup and reusable contact lenses with a history of eczema is (or will soon become) already a DED patient. A suspicious optic nerve get’s a glaucoma work-up, so why does the dry eye patient deserve anything less? Tear film analysis and meibography are critical to staging the disease…and like glaucoma, the symptoms can be silent!
There it is -Some (certainly not all) of my learnings after spending over 600 clinical hours in the last 2 years at the dry eye clinc treating this challenging condition and the patients that live with it. Confidence in understanding the physiology of dry eye disease allows the lessons of the failure of one patient to be the success of the next.
In good health,
Dr. Richard Maharaj OD, FAAO
Cinical Director,
eyeLABS Optometry and Center for Ocular Surface Disease
twitter: @eyelabsinc
info@eyelabs.ca